Thinking, reasoning, and independent function are all negatively impacted by dementia with Lewy bodies (DLB), a form of progressive dementia. It may exhibit REM sleep behavior disorder, recurrent visual hallucinations, spontaneous changes in attention and alertness, slow movement, tremors, or rigidity.
Patients with Lewy body dementia are more likely than AD dementia patients to die from respiratory causes and frequently die from dementia-related complications. Continue reading to find out more.
What is Lewy Body Dementia (LBD)?
The condition known as Lewy body dementia (LBD) is characterized by abnormal accumulations of the protein alpha-synuclein in the brain. The chemicals in the brain are impacted by these deposits, known as Lewy bodies, and these modifications can result in issues with thought, movement, behavior, and mood. One of the most typical causes of dementia is Lewy body dementia.
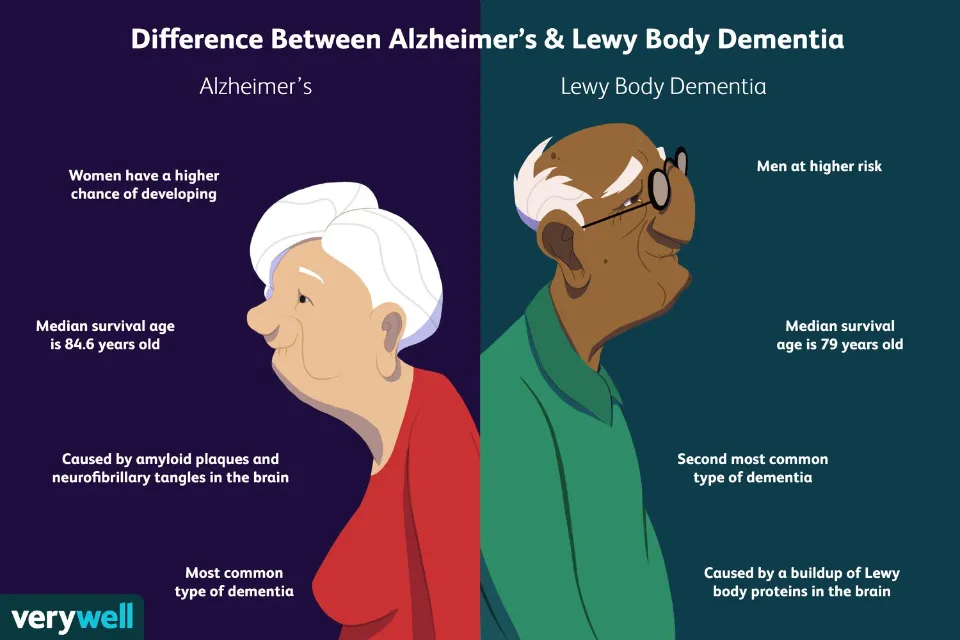
In the United States, LBD affects over 1 million people. Although occasionally younger people have LBD, people typically begin to exhibit symptoms around the age of 50. LBD seems to affect slightly more men than women.
It can be difficult to diagnose LBD. Early LBD symptoms are frequently mistaken for those of other brain diseases or psychiatric disorders that share some of the same symptoms. Lewy body dementia can develop by itself or in concomitance with other brain disorders.
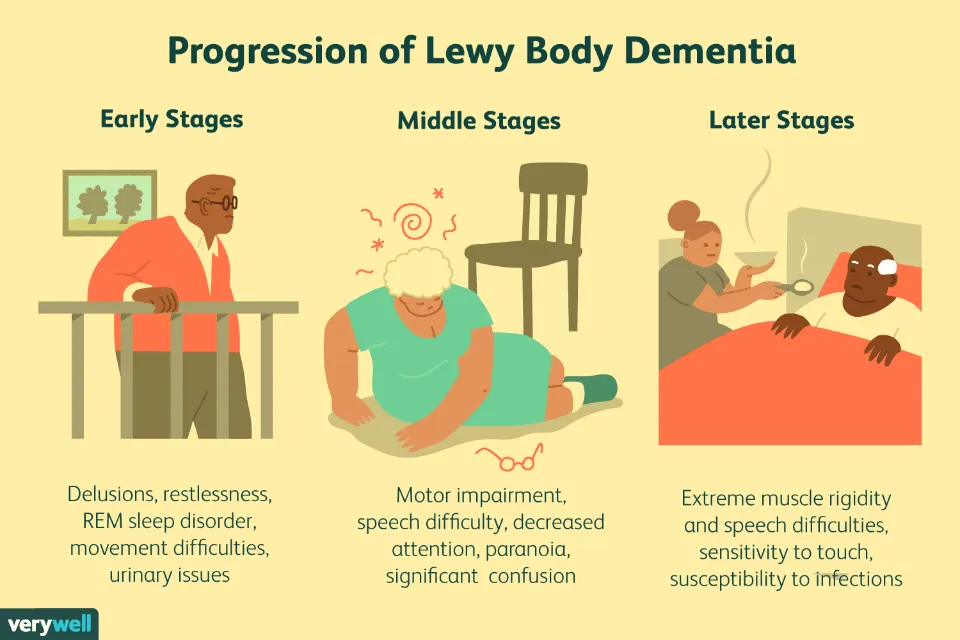
Since the illness is progressive, its symptoms develop gradually over time. From the time of diagnosis until death, the disease lasts an average of five to eight years, but for some people, that time period can be as long as twenty. Individual differences in symptom severity, age, and general health greatly influence how quickly symptoms appear and change.

People can function largely normally in the early stages of LBD because symptoms may be mild. People with LBD become more dependent on assistance as the disease worsens because their cognitive and motor skills deteriorate. They frequently require only other people’s help and care in the later stages of the illness.
For a while, some LBD symptoms may improve with treatment. The disease is currently incurable. Research is advancing our knowledge of this difficult condition, and technological developments may someday result in better diagnostic tools, better patient care, and novel therapeutic approaches.
Symptoms of Lewy Body Dementia
Core symptoms of dementia with Lewy bodies include:
- alterations in reasoning and thinking.
- erratic cognition with delirium-like symptoms.
- persistent, well-formed visual hallucinations.
- acting out dreams is a REM sleep behavior disorder.
- spontaneous parkinsonism with rigidity, tremor at rest, or slowness of movement.
Other symptoms may include:
- difficulty understanding visual data.
- Malfunctions of the “automatic” (autonomic) nervous system, which controls automatic functions of the body, such as sweating, blood pressure, heart rate, digestion and sexual response.
- Potentially serious memory loss that is less obvious than Alzheimer’s.
Differences Between Alzheimer’s and Lewy Body Dementia
- Memory loss is typically a symptom that is more noticeable in early Alzheimer’s than in early DLB. However, in addition to its more typical effects on judgment, planning, and visual perception, advanced DLB may also result in memory issues.
- Compared to Alzheimer’s, DLB movement symptoms are more likely to be a major early cause of disability. The moderate and severe stages of Alzheimer’s, however, can result in issues with walking, balance, and mobility.
- Compared to Alzheimer’s, early-stage DLB has a significantly higher incidence of hallucinations and misidentification of familiar faces.
- As opposed to Alzheimer’s, early DLB is more prone to REM sleep disorder.
- Compared to Alzheimer’s, early DLB is much more prone to autonomic nervous system disruption, which can result in symptoms like a drop in blood pressure upon standing, vertigo, falls, and incontinence.
Treatment and Care for Lewy Body Dementia
While LBD cannot currently be prevented or cured, some symptoms may temporarily improve with treatment. Medication, physical and other forms of therapy, and counseling may all be included in an LBD treatment plan. Making a plan to identify any equipment and update your home’s security can simplify daily tasks.
A knowledgeable care team can frequently recommend ways to enhance quality of life for both people with LBD and their caregivers.
Building a Lewy Body Dementia Care Team
A neurologist with expertise in movement disorders and/or dementia may be of assistance to a person with LBD after they have been diagnosed. To carry out your treatment plan, your primary care physician can collaborate with other experts. Physical, speech, and occupational therapists, as well as mental health and palliative care experts, may be useful depending on a person’s specific symptoms.
Another useful tool for LBD patients and their caregivers is support groups. People can find workable solutions to everyday problems and receive emotional and social support by exchanging experiences and advice with others facing similar challenges.
Lewy Body Dementia Medications
For the treatment of LBD symptoms, a number of medications and other options are available. Because some medications can exacerbate some symptoms, it is crucial to work with a skilled healthcare provider.
Coping With Cognitive Changes
Treatment for the cognitive symptoms of LBD may involve using some of the same drugs that are used to treat Alzheimer’s disease. These medications, referred to as cholinesterase inhibitors, work by inhibiting a brain chemical crucial for memory and thought. They might also lessen delusions, apathy, and hallucinations. One Alzheimer’s medication, rivastigmine, has been authorized by the U.S. Food and Drug Administration to treat cognitive symptoms in dementia caused by Parkinson’s disease. A number of additional medications are undergoing testing to see if they can treat the symptoms of LBD or stop the underlying disease process.
Managing Sleep Disorders in Lewy Body Dementia
Sleep issues can make caring for someone with LBD more difficult and may worsen their confusion and behavioral issues. A doctor can request a sleep study to find out if there are any hidden sleep disorders, like sleep apnea, restless legs syndrome, or REM sleep behavior disorder.
Acting out one’s dreams is a common LBD symptom of REM sleep behavior disorder, which can cause insomnia and even harm to sleep partners and individuals. At very low dosages, the medication clonazepam, which is used to treat panic attacks and control seizures, is frequently effective for the disorder. However, it may also cause adverse reactions like lightheadedness, shakiness, and cognitive difficulties. When taken alone or with clonazepam, the hormone melatonin, which is produced naturally and is used to treat insomnia, may also have some advantages.
In LBD, excessive daytime sleepiness is also typical. If it gets bad enough, a sleep expert might recommend a stimulant to help the person stay awake during the day.
Some LBD sufferers have trouble drifting off to sleep. A doctor might suggest taking a prescription medication if you consistently have trouble falling asleep at night. It is crucial to remember that treating insomnia and other sleep issues in people with LBD has not been thoroughly researched, that treatments may make daytime sleepiness worse, and that they should only be used with extreme caution. Increased daytime exercise, avoiding late-day caffeine, alcohol, and chocolate consumption, as well as avoiding lengthy naps, are other ways to deal with sleep issues.
Summary
In light of this, Lewy body dementia has the potential to result in death, just like dementia does, as the accompanying symptoms worsen.