Your joints are intricate anatomical structures. As a result, it may be difficult to identify the cause when you start experiencing joint pain. Bursitis and arthritis are two of the most prevalent medical conditions that can result in joint pain, and because they both exhibit similar symptoms, it can be challenging to tell them apart without the aid of a medical professional.
Bursitis and arthritis are two distinct conditions with some similarities. Rheumatoid arthritis (RA) and osteoarthritis (OA), two of the most prevalent chronic diseases, are included in the category of arthritis. Usually brought on by overuse, trauma, or infection, bursitis is a transient condition. Both involve discomfort, pain, and joint inflammation.
Please read this article to learn more about arthritis and bursitis.
What Is Bursitis?
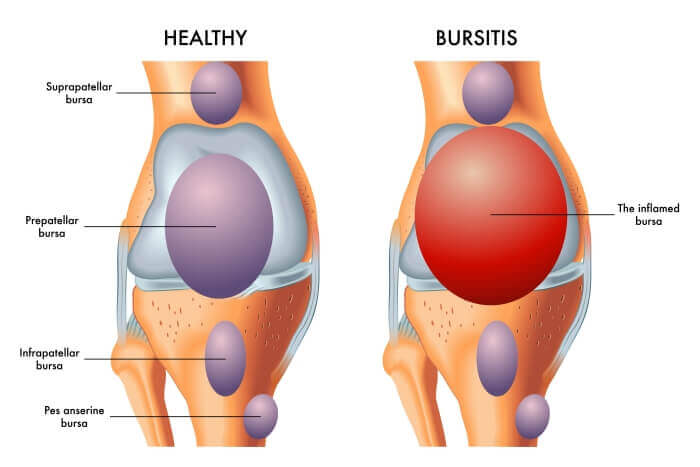
The fluid-filled sacs called bursae, which are located close to the joints, become inflamed in bursitis. To lessen joint friction and inflammation, the bursae serve as cushions between bones, tendons, and muscles. They might become swollen as a result of overuse, protracted postures, or inflammatory conditions.
As a person gets older, their risk of developing bursitis rises. Sports, manual labor, and playing an instrument all involve repetitive motions and pressure on specific joints, which can raise the risk.
Additionally, pressure on particular body parts, such as when kneeling, can raise your risk of developing bursitis. Bursitis can also be caused by medical conditions like thyroid disease, gout, diabetes, and arthritis. Bursitis can occasionally be brought on by a sudden injury or infection.
Activities that can lead to bursitis include:
- Carpentry
- Gardening and raking
- Painting
- Scrubbing
- Shoveling
- Sports—like tennis, golf, and baseball
- Bad posture or a joint that’s not well-positioned
- Different leg lengths, bone spurs, or other musculoskeletal structural issues
What Is Arthritis?
A family of medical conditions known as arthritis typically manifests as joint pain, stiffness, and swelling. Rheumatoid arthritis, an auto-immune condition in which the immune system attacks joint tissue, and osteoarthritis, which is brought on by the deterioration of the cartilage in joints, are two of the most prevalent types of arthritis. You may be interested in Does Rheumatoid Arthritis Cause Hair Loss?
It’s critical to seek medical attention as soon as you suspect you may have arthritis. Since arthritis worsens over time, getting a diagnosis early will allow you to start treatment right away. The majority of forms of arthritis have no known cure, but with the right medical care, you can control your symptoms and slow the disease’s progression.
Patients with arthritis who are not properly treated may experience joint degeneration, which can cause increased pain, loss of joint function, joint deformation, and disability. Depending on the type of arthritis, there are various treatment options, including drugs, physical therapy, injections, and dietary changes.
In order to lubricate the arthritic joint and reduce inflammation, your doctor may also inject certain substances into it. Modern treatments like stem cells have also demonstrated promising outcomes in the regeneration of cartilage.
The Similarities Between Arthritis And Bursitis
Bursitis and arthritis share a number of similarities. It can be challenging to distinguish between the conditions because of their similar bodily locations and numerous overlapping symptoms.
Symptoms
Both conditions can cause:
- Pain and aching in joints
- Stiffness
- Swelling
- Redness
- Tenderness to touch
Locations
The conditions also affect similar locations, including:
- Shoulders
- Knees
- Wrists
- Hips
They both also have the capacity to have an impact elsewhere.
The Differences Between Arthritis And Bursitis
Most people cannot tell the difference between arthritis and bursitis in the early stages. Both conditions share symptoms like joint pain, stiffness, swelling, and redness. The wrists, shoulders, knees, and hips are among the joints where arthritis and bursitis can develop; bursitis is more likely to affect larger joints, whereas some types of arthritis first manifest in smaller joints, such as the fingers or toes. There are some key distinctions between the two conditions, including:
- Mechanism—while arthritis attacks the principal joint tissue like the cartilage, bursitis affects only the bursae.
- Onset—arthritis tends to appear gradually and progressively worsens, but bursitis may appear suddenly after an injury or intense period of activity.
- Duration—bursitis is an acute condition that typically resolves on its own after a few weeks of rest, while arthritis will worsen over time if not properly managed.
Risk Factors For Bursitis
Bursitis can affect anyone, but certain circumstances increase the likelihood. You’re more likely to develop bursitis if you:
- Are over age 40, as risk increases with age
- Participate in sports or activities that repeatedly strain an area of the body where you have a bursa, such as your shoulder
- Are a “weekend warrior” when it comes to exercise. Bursitis frequently results from being mostly sedentary followed by an abrupt overload, claims Dr. Huffstutter.
- Are overweight, since excess weight puts pressure on the bursa, as well as the joints themselves)
- Have arthritis. Both conditions frequently overlap because they both relate to the joint or, in the case of the bursa, a structure that lubricates the joint. Bursitis risk may be increased by a number of forms of arthritis, including gout, RA, and OA.
The majority of these arthritis-related risk factors also apply to bursitis. For instance, OA may manifest years after years of physical activity that wears down cartilage, and RA is typically diagnosed in middle age. Along with other types of arthritis, such as RA, OA, and gout, overweight people are more likely to develop them.
Between Bursitis And Arthritis, How Can You Tell The Difference?
Finding the source of your joint pain might be challenging. Given that the immediate symptoms of the conditions can be very similar, a doctor will probably be necessary to diagnose your condition. Bursitis may cause intermittent joint pain, whereas osteoarthritis (OA) may cause more persistent pain.
If you experience the recent onset of symptoms following a repetitive motion activity, such as playing tennis or crawling on your hands and knees, you should take bursitis into consideration.
Your body’s joints may experience RA symptoms at various locations. Rheumatoid nodules are skin nodules that occasionally accompany the usual joint swelling in rheumatoid arthritis.
Diagnosing Your Pain
To rule out potential dangers, it’s crucial to see a doctor as soon as you notice joint pain. To rule out much more serious conditions like rheumatoid arthritis or cancer is crucial. It may turn out to be bursitis, which can be treated with targeted therapies or rest.
The initial procedure when you see a doctor is a thorough history and physical. A thorough history should cover your work and/or exercise routines, your family’s medical history (including any chronic illnesses they may have, such as arthritis), and the events leading up to the pain. Exercises to test your range of motion and pain symptoms might be required of you.
Your doctor may order additional tests if the physical examination is inconclusive. A thorough evaluation, which may include blood tests and medication trials, may be necessary if your doctor suspects an autoimmune disease like rheumatoid arthritis.

For verification of bursae inflammation, an ultrasonogram or straightforward injection may be required. An x-ray or MRI may be prescribed to confirm the diagnosis of arthritis if your doctor suspects it to be that condition.
If the condition is bursitis, your doctor will likely advise resting the joint unless it is brought on by another condition like diabetes, gout, or infection. Your doctor will work with you to create a multimodal treatment plan if your joint pain is due to arthritis, which may include prescription drugs, lifestyle modifications, injections, and physical therapy.
Treatments Of Arthritis And Bursitis
Both the treatments and the results of all of these conditions vary. Discover how to treat RA, OA, and bursitis by reading the information below.
Bursitis
Many at-home remedies, over-the-counter (OTC) medications and interventions from a doctor or specialist can all be used to treat this condition.
First-line treatment for bursitis may include:
- applying ice and heat to the affected joint
- resting and avoiding repetitive movements in the affected joint
- performing exercises to loosen the joint
- adding padding to sensitive joints when engaging in manual activities
- wearing a brace or splint to support the joint
- taking OTC medications like nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, to manage pain and reduce swelling
Your doctor might suggest physical or occupational therapy, stronger oral or injectable prescription drugs, or surgery if the symptoms don’t go away with these treatments.
The fact that surgery is rarely advised should not be overlooked.
Osteoarthritis
Instead of attempting to treat OA, treatment will concentrate on symptom reduction and function preservation. Your doctor may recommend:
- medications, including OTC and prescription drugs, including topicals
- exercise and other activities
- lifestyle modifications, like avoiding repetitive activities and managing your weight
- physical and occupational therapy
- braces, splints, and other supports
- surgery, if symptoms are very debilitating
Rheumatoid Arthritis
If you have RA, your physician may advise treating joint pain as it develops. To prevent flare-ups and maintain remission, however, treating RA necessitates a variety of management techniques.
Remission denotes the absence of active symptoms and the presence of typical inflammatory markers in the blood.
The use of NSAIDs or other painkillers and anti-inflammatory drugs may be part of the management of joint pain. Your doctor might also advise resting the joints while continuing to be active in other ways.
Prescription drugs like biological response modifiers and disease-modifying antirheumatic drugs may be used in the long-term management of RA.
In order to prevent the condition from developing and experiencing joint pain, your doctor may also advise you to avoid stress, maintain an active lifestyle, eat healthily, and give up smoking, if you do.
Does Bursitis Lead To Arthritis?
Arthritis is not a result of bursitis. Although having arthritis increases the likelihood of developing bursitis, the opposite is not true either.
They are frequently spotted together. For instance, if a person has shoulder arthritis, they may alter how they use their shoulder, which may result in bursitis. Altering their gait and irritating the bursa in that region, people may also develop arthritis in their knee or hip.
When To See A Doctor?
Visit your doctor if your joint pain lasts more than a few weeks. You should see a doctor right away if you:
- become unable to move your joint
- notice the joint is very swollen and the skin is overly red
- experience severe symptoms that interfere with your ability to complete daily activities
If you have joint pain and fever or other flu-like symptoms, you should also visit your doctor. An infection could be the cause of a fever.
The Bottom Line
There are numerous illnesses that can lead to joint pain. OA and RA cause more persistent joint pain than bursitis, which is typically a temporary condition. It is best to seek medical attention as soon as possible in order to control these conditions, such as bursitis or arthritis. Bursitis will recover quickly with treatment, and arthritis will progress more slowly.



