Urinary incontinence and some kinds of poisoning are just two of the conditions that anticholinergics can treat. Due to decreased urination, digestion, and mucus and salivary secretion, they may have side effects.
Learn more about anticholinergic side effects in the following paragraphs, as well as how to avoid them.
What Are Anticholinergic Drugs?
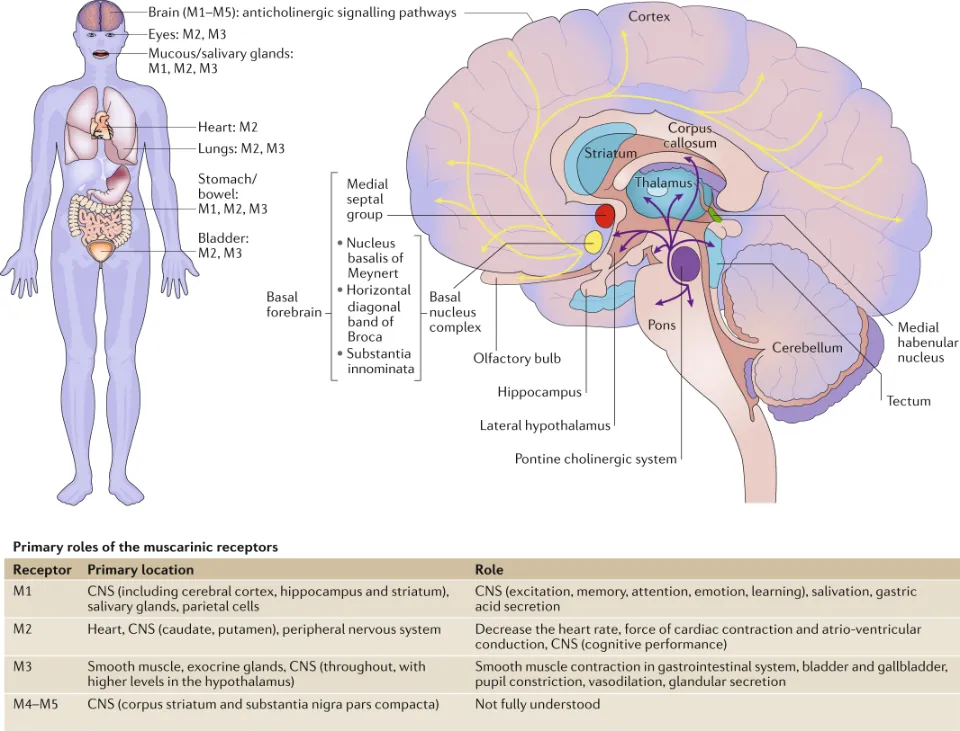
Anticholinergic medications can cause issues, especially for elderly people. Acetylcholine’s function as a neurotransmitter is blocked (antagonized) by anticholinergic medications. When nerve cells need to communicate with other cells, they release a chemical called a neurotransmitter. Acetylcholine is a neurotransmitter that affects learning and memory in the brain as well as muscle contractions in the body.
Drugs with anticholinergic properties have been used in medicine for many decades in the treatment of such diverse conditions as:
- Diarrhea
- Asthma
- Overactive bladder (OAB) and urinary incontinence
- Chronic obstructive pulmonary disease (COPD)
- Surgery and anesthesia for muscle relaxation
- Gastrointestinal disorders
- Insomnia
- Motion sickness
- Toxicity of certain poisonings
- Parkinson’s disease symptoms
- Psychiatric disorders
Benefits of the Anticholinergic Effect
Many medications work toward their therapeutic objectives due to the anticholinergic effect. A person may get relief from diarrhea, for instance, by slowing bowel movements.
Similarly, the breathing restriction associated with asthma and COPD can be improved when the cholinergic receptors of the lungs are blocked.1
Antispasmodics—drugs that temper muscle spasms related to gastrointestinal and other issues—are one class of drugs in which the anticholinergic effect is considered beneficial.2
Antispasmodic drugs with an anticholinergic effect include:
- Bentyl (dicyclomine)
- Buscopan (hyoscine butylbromide)
- Levsin (hyoscyamine)
- Lomotil (atropine/diphenoxylate)
- Enablex (darifenacin)
- Pamine (methylscopalamine)
- Spiriva (tiotropium bromide)
- Symmetrel (amantadine)
- Vesicare (solifenacin)
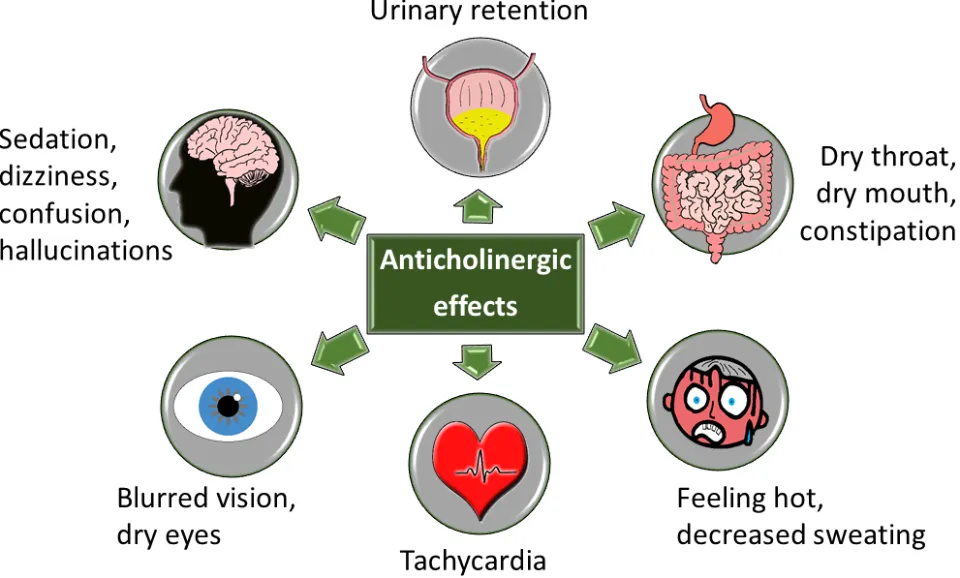
Types of Anticholinergic Side Effects
Peripheral and central side effects of anticholinergic drugs can be distinguished from one another. In order to treat patients effectively, doctors must be aware of the potential for these side effects. Anticholinergic side effects have significant potential for medical complications, and in susceptible patients—especially older patients or patients with a preexisting condition like asthma—these side effects can be crippling.
Peripheral Side Effects
Because they are more physically manifested than central side effects, peripheral side effects could be simpler to identify. Dry mouth, constipation, urinary retention, bowel obstruction, dilated pupils, blurred vision, elevated heart rate, and decreased sweating are among the typical symptoms.
Physicians should exercise caution despite the fact that not all peripheral side effects seem severe because they can result in a wide range of medical complications. There are many different types of complications, such as myocardial infarction, gum ulcers, and respiratory issues.
Central Side Effects
Cognitive dysfunction has long been acknowledged as being at the heart of the abnormalities in schizophrenia. By having central side effects brought on by anticholinergic properties of antipsychotic drugs, this preexisting impairment may become worse. Concentration problems, confusion, attention problems, and memory problems are some of the cerebral side effects of central administration.
Side effects can occur even when this medication is used properly. Anticholinergics’ potential side effects can vary depending on the medication and dosage you’re taking.
Side effects can include:
- Dry mouth
- Blurry vision
- Constipation
- Drowsiness
- Sedation
- Hallucinations
- Memory problems
- Trouble urinating
- Confusion
- Delirium
- Decreased sweating
- Decreased saliva
How to Prevent Anticholinergic Side Effects?
Anticholinergic side effects can be easily managed, but occasionally something may happen that requires extra care.
Decrease the Dose of the Antipsychotic
A doctor’s first course of action is to reduce the antipsychotic’s dosage. Sometimes dose reduction can lessen the anticholinergic effects. Changing to an antipsychotic with a lower anticholinergic profile can also stop the symptoms from persisting. While data9 have demonstrated the differences in vitro among the antipsychotics, whether or not these differences translate to clinical activity is subject to debate.
Eliminate Or Reduce the Doses of Other Medications
Another option is to stop using or reduce the dosage of additional medications that are known to have negative side effects on cholinergic receptors. Multiple medications are frequently prescribed to patients, especially those who are elderly. Blazer and colleagues conducted a study of the potential for anticholinergic toxicity among long-term care residents. Drug administration and drug quantity were asked about from participants 65 years of age and older who had stayed in a nursing home continuously for a year. 60% of the 5902 nursing home patients received medications with anticholinergic properties, and 565 patients may have taken three or more anticholinergic drugs. It is possible to lessen the risk of adverse anticholinergic effects by being aware of the medications a patient is taking and removing any that are unnecessary.
Conclusion
Acetylcholine is a neurotransmitter that is inhibited by anticholinergic medication. This blocks the nerve impulses that cause uncontrollable muscle contractions and other bodily functions.
Speak with your healthcare provider if you are suffering from intolerable side effects brought on by a drug’s anticholinergic effects. Depending on your healthcare provider, the practitioner might be able to reduce the dosage or come up with a suitable replacement.
FAQs
How Do You Detox from Anticholinergics?
Reduce dose by 50% every 1 to 2 weeks. Stop taking the medication when you have reduced it to 25% of the initial dose and no signs of withdrawal remain. Approximately 75% of the previously tolerated dose should be used if any withdrawal symptoms appear.
How Long Does Anticholinergic Syndrome Last?
When taken in excess, atropine and scopolamine can result in anticholinergic syndrome. The anticholinergic toxicity usually occurs within 30–60 min after consumption of the plant, and the symptoms can last for 24–28 h due to delayed gastric emptying caused by the anticholinergic alkaloids.



