Possible Causes of Long COVID
Although four potential explanations for Long COVID’s causes have surfaced, it is important to note that this research is still in its early stages.
Danny Altmann, an immunologist at the Imperial College London, told Nature last August, “In reality, if you were to imagine the long COVID at this particular time as being somewhat “Wild West” and hopeless.” He added that “we’ve now got little scattered bits of evidence. We’re all scurrying to try to reach some sort of agreement. We are so far removed from that. It is very unsatisfactory.”
Some scientists believe Long COVID may actually be a number of syndromes because it has 200 symptoms on average and is known to affect every system in the human body.
Jennifer Couzin–Frankel, a staff writer on biomedical and clinical research for the journal Science, explained the complex process of Long COVID research in an article last June:
Untangling the complex syndrome, with a definition that is still in flux, is a laborious, step-by-step process for each of these researchers, as well as many others looking into the causes of Long Covid. To begin with, they need to demonstrate that a potential factor—like minute clots, lingering virus, or immune abnormalities—occurs disproportionately in people with Long Covid. The challenging part now is to demonstrate how each of these characteristics, individually or collectively, contributes to the coronavirus’s ability to transform millions of people into shadows of their former selves.
The likelihood of creating efficient treatments is slim without knowledge of the condition’s underlying cause. Though the research being done now is addressing a moving target, some new information has been discovered.
The four theories for the potential causes of Long COVID are blood microclots, immune dysfunction, the virus’s long-term persistence, and dysbiosis of the gut microbiome (disruption of the gut’s typical microorganisms). Studies are still in their very early stages, and it’s likely that after more investigation, additional factors will become apparent.
Speaking at an online forum last August hosted by Knowable Magazine, Akiko Iwasaki, a Long COVID advocate, immunologist and professor of immunobiology at Yale School of Medicine, explained that the four causes “are not mutually exclusive. These things can also be combined in people.”
Persistent Virus
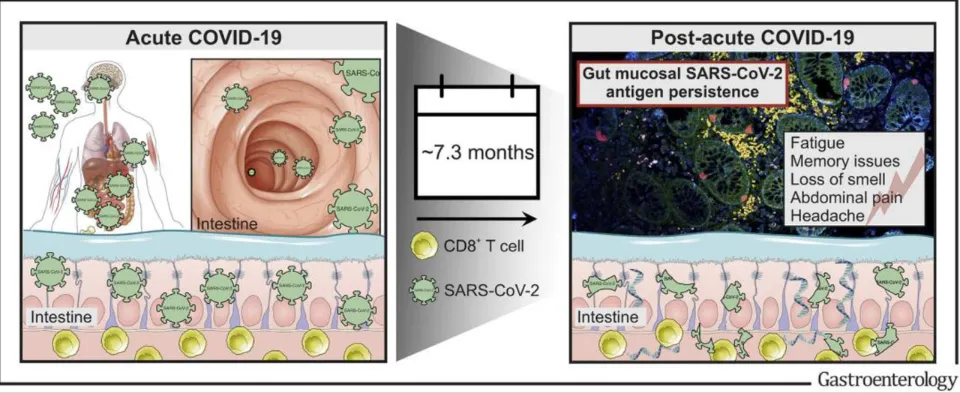
The SARS-CoV-2 virus is showing signs of persistence and ongoing replication in the body long after the initial infection.
The results of a study by researcher Daniel S. At the University of California’s Critical Care Medicine Department, Chertow and his team discovered virus in the brain, lung, muscle, and gut tissues. They discovered proof that the virus was propagating.
The SARS-CoV-2 virus can remain in the gut for a while, according to a number of studies. In an article published last May in Nature, oncologist and geneticist Ami Bhatt of Stanford Medicine referred to the persistent bits of virus as “ghosts.”
GI (gastrointestinal) symptoms like nausea, vomiting, and diarrhea were reported by 11–18% of COVID-19 hospitalized patients. A paper published last April by senior research scientist at the Department of Genetics at Stanford University Aravind Natarajan and his team reported that “gastrointestinal symptoms and fecal shedding suggests prolonged gastrointestinal infection” and that there was persistent evidence of GI tract RNA from SARS-CoV-2.
The paper stated:
Furthermore, prolonged presence of SARS-CoV-2 in the GI tissue may also have an impact on the hitherto mysterious phenomenon of post-acute sequelae of SARS-CoV-2 infection (PASC) or “Long COVID,” where individuals suffer from an unusual constellation of symptoms even after recovery from the respiratory All things considered, it is crucial that we comprehend whether or not the GI tract is infected as well as the dynamics of the infection in this tissue, both in terms of the acute infection and the long-term effects of COVID-19.
In a study released in May of last year, gastroenterologist Herbert Tilg and his colleagues at the Medical University of Innsbruck looked at 46 patients, 21 of whom had at least one Long COVID symptom, who had a COVID-19 infection an average of 219 days before their endoscopy. According to polymerase chain reaction analysis, 31% of the patients had viral RNA that could be detected in their biopsy specimen, and 70% of the patients had SARS-CoV-2 present.
The authors stated:
We offer proof that SARS-CoV-2 antigen persistence in the gut is a contributing factor to the immune system’s disruption in postacute COVID-19. To combat this rapidly spreading disorder around the world, more clinical trials should be conducted to determine whether viral antigen persistence (in and outside the gut) underlies the pathophysiology of post-acute COVID-19.
“Our paper is a clinical observation and doesn’t prove that lingering virus is harming people,” Tilg commented to Science.
Microclots
Etheresia Pretorius, a physiologist at South Africa’s Stellenbosch University, and Douglas Kell, a systems biologist at the University of Liverpool, have been the main proponents of the microclot hypothesis. The #teamclots hashtag on Twitter has been used to promote the microclot theory.
After the COVID-19 pandemic struck in 2020, Pretorius and Kell brought forward their earlier work on clotting disorders. “We thought to look at clotting in COVID, because that is what we do,” Pretorius told Nature.
Pretorius and Kell compared individuals who had recently contracted COVID-19, Long COVID patients, and an uninfected cohort as a control group while examining fibrin, a protein linked to clotting. In contrast to what they had previously observed in other inflammatory diseases like diabetes, they discovered that there was more clotting.
Another study led by Pretorius published last August in the journal Cardiovascular Diabetology examined blood from 80 patients on a South Africa has a lengthy COVID register. In addition to extremely high levels of platelet activation (blood components that regulate clotting), the study discovered evidence of microclotting in all of the blood samples.
The study noted, “Endothelial damage might be one of the primary causes of persistent Long COVID/PASC symptoms, along with platelet pathology and the presence of microclots in the circulation.”
A comment by Pretorius published in The Guardian in January 2022 stated:
Cellular hypoxia, which occurs when cells do not receive enough oxygen in the tissues to maintain bodily functions, is caused by the presence of persistent microclots and hyperactivated platelets (also involved in clotting). The numerous reported incapacitating symptoms could all be related to widespread hypoxia.
What causes microclots to form is not fully understood. Pretorius and Kell believe that the virus’s use of the spike protein to enter the host cell may have an effect on the development of microclots. Pretorius and Kell’s study showed that the SARS-CoV-2 spike protein added to blood caused clotting.
A paper published in Bioscience Reports by researcher Lize M. Grobbelaar at the Department of Physiological Sciences at Stellenbosch University stated:
[We [produce evidence for spike protein’s significant contribution to the hypercoagulability (hyperclotting) observed in COVID-19 patients. Both purified fluorescent fibrinogen (a blood plasma protein) and PPP (platelet-poor plasma) from healthy individuals experience abnormal clotting; the clots’ composition was revealed to be amyloid (a protein aggregate linked to various diseases), which causes abnormal clotting in both of these samples.
Researchers have identified potential remedies. According to Pretorius and Kell, some patients with Long COVID may experience symptom relief when receiving treatment with a combination of two antiplatelet therapies and an anticoagulant. Because they can result in excessive bleeding, these treatments need to be closely monitored. Blood filtering via a procedure called apheresis has been attempted, with some encouraging outcomes.
Given that it is based on a small number of studies, the microclot theory has come under fire. Other researchers have failed to find microclots after COVID-19 infection.
Alex Spyropoulos, a haematologist at the Feinstein Institutes for Medical Research in New York, told Nature that the microclot hypothesis presents “a very elegant mechanism” but that much more work is needed to tie the lab markers to clinical symptoms. “What’s a little bit disturbing is that these authors and others make huge leaps of faith,” Spyropoulos said.
Immune System Gone Haywire
The immune system becoming overactive and attacking healthy proteins as a result of the body’s continued presence of SARS-CoV-2 RNA is another popular theory regarding Long COVID.
In a comment in the Los Angeles Times last August, Eric Topol noted the following immunological processes that could explain Long COVID:
Exhausted T-cells, which are immune system cells that fight foreign invaders, antibodies that target the body’s own proteins, markers of reactivation of previous herpes virus infections, such as Epstein-Barr virus and varicella-zoster virus (which causes chicken pox), and antibodies to the virus’ spike protein.
Early in the pandemic, researchers observed that dangerous inflammation—the so-called cytokine storm—was probably caused by an agitated immune system that could cause death and tissue damage.
Last August, immunologist Matthew Woodruff and his team at Emory University published a research paper in the journal Nature which found that some patients developed antibodies to fight their The COVID-19 infection attacked body organs and tissues as a result.
Woodruff stated, “We also demonstrate that Long COVID-19 patients can have self-directed antibodies that last for months or even years.”
The immune system’s interaction with the tissues in its own body is a very intricate process. Normally, when a pathogen enters the body, naïve B cells are produced. It can take up to a fortnight for these cells to go through a program that teaches them how to recognize and combat a particular invader. In the event of a severe infection, this process may fail, causing the antibodies to attack the body. These aberrant antibodies can survive for months, as evidenced by the work of Woodruff and others.
Woodruff commented, “Additionally, in ongoing research that has not yet undergone peer review, we discover that these responses are not only present in patients who are recovering from severe illness but are also easily discernible in a sizable subset of Long COVID-19 patients who were recovering from more mild illnesses.”
Dr. T-cell immunologist was one of the first and most persistent scientists to raise concerns about COVID-19’s potential to harm the immune system. Anthony Leonardi spoke in-depth with the WSWS twice about these and other pandemic-related subjects in the months of November and December 2021.
Dysbiosis of Microbiome Or Disruption of Gut Micro-organisms
In the human gut, there are trillions of microbes that are involved in maintaining general health. Bacteria, viruses, fungi, and archaea (organisms that are somewhat related to bacteria) are known to reside in the gut.
The microbiome and its human host coexist normally. According to a June 2021 article published in Frontiers in Microbiology by microbiologist Amy D. Proal of the PolyBio Research Foundation, “These host microbiome/virome communities persist in a state of balance or homeostasis when the body is healthy because a strong host immune response keeps them “in check.””
According to a theory, a SARS-CoV-2 infection might disturb the microbiome and trigger the reactivation of dormant pathogens.
“It’s also possible that there are latent viruses that are reactivated to cause some of these symptoms such as the Epstein-Barr virus,” Ikiko Iwasaki told Knowable Magazine. Chronic fatigue syndrome is thought to be brought on by the herpes virus Epstein-Barr.
An opinion piece by researchers Kai Hilpert and Ralf Mikut published in September 2021 in Frontiers in Microbiology reviewed the current literature demonstrating the impact of Intestinal microbiome and SARS-CoV-2.
The authors stated, “Due to increased inflammation and interactions between the oral, pulmonary, and gastrointestinal microbiomes, these modifications may result from an infection that has already spread to the gut.” They went on to observe that “some of the symptoms described in chronic Additionally linked to a dysbiosis of the gut microbiome are symptoms of COVID-19 syndrome (CCS), such as fatigue, sleep disturbance, joint pain, anxiety/depression, headache, and diarrhea.”
They also demonstrate the importance of the gastrointestinal tract in maintaining immune system homeostasis and the role of dysbiosis in causing inflammation and chronic symptoms.
Cures and Treatments
Long COVID has no known cure as the underlying cause is still a mystery to science. Although some treatments have been created, they have not yet been scientifically validated and can be viewed as an ad hoc method based on treating the numerous Long COVID symptoms.
A review of treatments by researcher Ho Cheng Koc and her team at the Centre of Reproduction, Development and Aging of the University of Macau stated, “Despite the release of several guidelines for Long COVID management, there is still a sizable practical gap. … In order to manage Long COVID, current clinical practice generally adopted a symptom-based approach.”
Numerous potential treatments put forth by scientists need more research. Antivirals like Paxlovid or Molnupiravir can be used to effectively target persistent viruses. Immunosuppressive drugs might be used if Long COVID is an autoimmune disease. Diet and probiotics may be used to treat microbiome dysbiosis.
Long COVID’s inflammatory effects have been treated with antihistamines, and dietary supplements like vitamins and minerals have also been used as anti-inflammatories. With varying degrees of success, antibody therapies like Infliximab, Tocilizumab, Siltuximab, Anakinra, and Leronlimab have been researched.
The understanding that Long COVID is a catch-all term encompassing a number of conditions may become clear with further study. Physician and heart disease researcher Chahinda Ghossein of Maastricht University commented that “the biggest obstacle that we are facing is we gave it one name, we gave it the name of The word “Covid” implies that there is only one disease. … All current studies demonstrate that it is not.”
Despite the fact that the research is still in its early stages and that other problems could materialize over time, it is obvious that more study is necessary to determine the exact causes of Long COVID. Even though the capitalist ruling elites around the world give lip service to the need for such research, they have restricted or refused to provide the funding required for it to move forward.
The Brookings Institute report cited above noted that the US government has allocated just $1.15 billion to study the disease, concluding “overall, the government’s record on supporting such work is poor.” It added, “as of 2021, the A second post-viral illness, ME/CFS, received less than $20 million a year from the NIH for research.”
The $1.15 billion allocated to the National Institutes of Health (NIH) in December 2020 for the study of Long COVID represents just 2.5 percent of the organization’s $45 billion annual budget and only 0.1 percent of the Biden administration’s historic $1 trillion military budget request for the upcoming year. Furthermore, the funding for Long COVID was a one-time allocation rather than an ongoing one.
Given the scope and difficulty of the issue, the British government allocated only £18.5 million in February for additional funding into Long COVID.
Nothing was allocated for Long COVID research in Australia’s first budget under the Albanese Labor government. This is despite the fact that since the government lifted all mitigation measures that slowed the spread of the virus, tens of thousands if not hundreds of thousands of Australians have contracted the condition.
Long COVID research funding is lacking as a result of the ruling elites’ general disregard for human life, which has been on full display for the past three years of the pandemic. While providing limitless resources to their military apparatus, there are to be no resources allocated to reducing the suffering of tens of millions of people around the world.
Governments’ reckless policy of simply denying the existence of the ongoing pandemic and failing to provide the necessary funding for Long COVID research are linked.



