The long-term effects of SARS CoV-2 infection, also known as Long COVID or post-acute sequelae of SARS-CoV-2 (PASC), continue to pose a serious threat to humanity three years after the COVID-19 pandemic. Long COVID researchers and advocates have correctly referred to the pandemic as a “mass disabling event,” which is ongoing and deepening despite all the lies and propaganda that “the pandemic is over.”
The enormous societal effects of the pandemic can be compared to an iceberg, where the short-term toll that Long COVID exacts is accompanied by the acute mortality and suffering that are visible on the surface but are frequently hidden but are nonetheless enormously large in numbers.
According to the Institute for Health Metrics and Evaluation (IHME), 6.73 million people have officially died as a result of 6.71 million people having the SARS-CoV-2 infection worldwide. Due to insufficient testing and data tracking systems in most nations, both numbers are well known to be vast undercounts. According to studies, COVID-19 has spread to most of humanity at this point, and the pandemic is responsible for over 20 million additional deaths.
An important recent scientific review, “Long COVID: major findings, mechanisms and recommendations” provided a conservative estimate that beyond these acute deaths, a staggering 65 million people are now suffering from Long COVID worldwide. The widely read paper, published in Nature Reviews Microbiology in The Scripps Research Institute’s Eric Jeffrey Topol and Julia Moore Vogel, along with Long COVID patient-researchers Hannah E. both Lisa McCorkell and Davis.
The researchers present a number of shocking statistics that demonstrate the criminality of what the ruling elites are wreaking on society. They note:
Long COVID is a condition that affects at least 65 million people worldwide, though the actual number is probably much higher given the large number of unreported cases. The incidence is estimated to be 10% of non-hospitalized cases, 50% of hospitalized cases, and 10% of cases who had received vaccinations. All ages and acute phase disease severity are associated with long COVID.
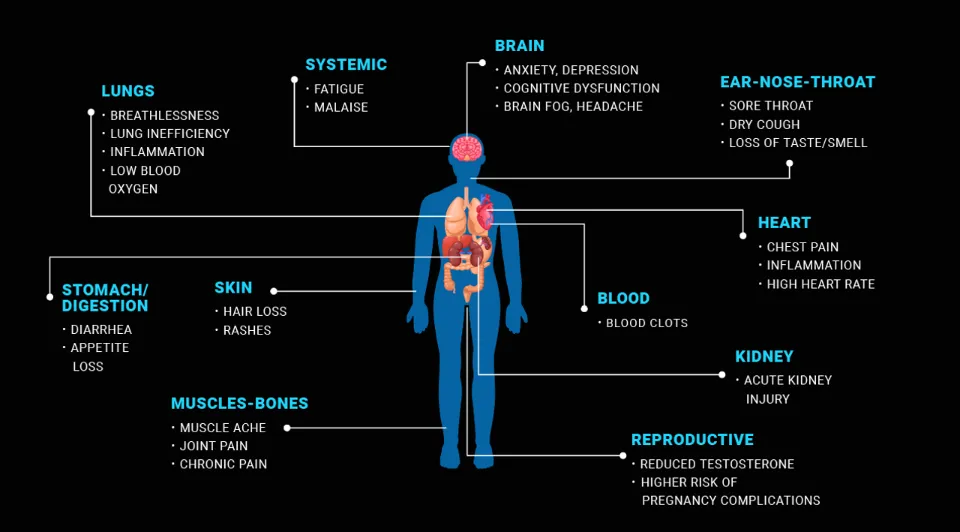
In part because it is linked to more than 200 symptoms that range from bothersome to incapacitating, Long COVID’s characteristics are still a mystery. Extreme fatigue, shortness of breath, pain when breathing, sore muscles, heavy arms or legs, ageusia (loss of taste) or anosmia (loss of smell), feeling hot and cold alternately, and tingling in the extremities are some of the most typical symptoms.
Every organ system in the body, particularly the cardiovascular, gastrointestinal, neurological, endocrine, respiratory, and genitourinary systems, can be attacked by COVID-19 and suffer long-lasting damage, according to studies cited in the Topol et al. review.
Significantly, COVID-19 can result in cardiovascular, thrombotic (clots), and cerebrovascular disease, type 2 diabetes, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and dysautonomia (dysfunction of the autonomic nervous system that regulates the body’s internal environment), particularly postural orthostatic tachycardia syndrome (POTS), which is characterized by an elevated heart rate when standing.
The authors draw the conclusion that these symptoms can linger for a few weeks, years, or even a lifetime, frequently making it impossible for sufferers to lead a normal life. The review states, “The number of people who have recently become disabled is a factor in labor shortages because a sizable portion of those with long COVID are unable to return to work. There are no proven effective treatments available right now.”
The immense social and medical impacts of Long COVID are the product of the homicidal “let it rip” mass infection policies that have now been implemented by every capitalist government throughout the world. One of the greatest crimes committed throughout the pandemic by capitalist politicians and the corporate media was the suppression and denial of Long COVID science, which was known to be a devastating illness from the very first wave of coronavirus.
It is obvious that Long COVID has accompanied each new wave of the pandemic and that it will continue to cripple a sizable portion of society for years to come. This review, as part of the World Socialist Web Site‘s The Global Workers’ Inquest into the COVID-19 Pandemic will detail the science and effects of Long COVID, the lessons that should have been learned from earlier post-viral illnesses, and the refusal of global capitalism to address this enormous and ongoing social catastrophe.
Identification of Long COVID
Patients who were unable to receive any effective treatment for Long COVID first recognized the condition for what it was. People who reported Long COVID symptoms during the initial wave in 2020 were frequently written off as suffering from a psychosomatic illness and ignored. This was despite the fact that Long COVID was entirely predictable because it is well known that bacterial and viral infections can have long-term effects that can manifest decades after the initial infection.
A comment published in Social Science & Medicine in October 2020, written by professor of Human Geography at the University of Glasgow, Felicity Callard, and Honorary Research Associate at University College London, Elisa Perego, stated, “Numerous heterogeneous and intricately developing symptoms were made visible by thousands of patients; however, in the early pandemic months, the majority of these symptoms were not frequently acknowledged within many healthcare and policy channels.”
According to the authors, social media was crucial in bringing together the expanding patient population globally and helping them spread awareness of their illness. “There are strong reasons to argue that Long Covid is the first illness to be made through patients finding one another on Twitter and other social media,” they stated.
Importantly, Callard and Perego dispelled the myth that COVID-19 is a contagious disease because patients were describing severe symptoms even at the beginning of the pandemic.
In an online post published in May 2020, Callard took up Britain’s Home Officer Deputy Science Advisor Rupert Shute’s assessment of COVID-19 as “mild.” She wrote, “As a patient, I have noticed that I resent the term “mild.” At a time when thousands continue to perish every day from a new and cruel disease throughout the world, the adjective may end up both revealing and concealing different logics.”
Perego recently spoke to the World Socialist Web Site. She is an ethical scientist urging the eradication of COVID-19 on a global scale.
Long COVID advocate, immunologist and professor of immunobiology at Yale School of Medicine, Akiko Iwasaki, related in an online forum last August in Knowable Magazine “Long COVID: A parallel pandemic” that in the early phase of the pandemic she investigated acute COVID-19, but that she often came across people who had lingering symptoms. She said:
We hadn’t expected such a large number of people to suffer serious illnesses. 50% of patients who are discharged from hospitals may still have chronic symptoms. While a mild or asymptomatic condition may result in a prevalence that is much lower but still in the 10 to 30 percent range. That is a sizable number of people.
How Many People Have Long COVID?
Most Long COVID victims are between the ages of 30 and 50, in relatively good health, and report only minor or no symptoms prior to infection. Since Long COVID does not have a single accepted definition, estimates of the condition’s prevalence vary greatly. Last year, Nature commented, “The definition and diagnosis of long COVID are not currently agreed upon.”
The World Health Organisation (WHO) published a “clinical case definition” in Neither patient advocates nor researchers have endorsed it as of October 2021. The condition is still defined by a variety of factors in academic studies.
An opinion piece published in August in The Conversation by According to research, 5 to 50% of people with COVID-19 infection also have Long COVID, according to Betty Raman, Associate Professor of Cardiovascular Medicine at the University of Oxford.
Aranka V.’s research group conducted a study with 76,422 participants. Ballering, MSc, found that “post-Approximately one in eight (12.5%) COVID-19 carriers in the general population may have a COVID-19 condition.”
According to a recent Brookings Institute report released in August, 2 million to 4 million working-age adults have reportedly left the labor force in the US alone as a result of Long COVID. According to the National Center for Health Statistics, approximately 16 million Americans who are working age (18 to 65) have Long COVID, or about 8% of this group.
A study published last July by the Reserve Bank of Minneapolis, “Long Haulers and Labour Market Outcomes,” estimated that out of the people they surveyed with Nearly 26% of respondents to the Long COVID had either quit their jobs entirely or cut back on their hours (by at least 10 hours per week on a basis of a 40-hour work week).
According to the British Trades Union Congress (TUC), 20% of people with Long COVID were no longer employed, and another 16% reported working fewer hours. Research published in The Lancet in According to a July 2021 study on a global cohort, 45 percent of Long COVID patients had to cut back on their hours and 22% of patients could no longer work due to ill health.
The Impacts of Long COVID on the Nervous System
One of the most common Long COVID symptoms is “brain fog,” which some COVID has long been used as a catch-all term for brain damage, according to its supporters. Three months after the initial infection, 20–30% of patients and 65–80% of those with more severe symptoms report having brain fog. This kind of cognitive impairment, which is difficult to think or concentrate on, can occur even in people who have no symptoms or only mild symptoms during their initial infection.
The detrimental effects of brain fog are severe. An article published last September in The Atlantic, “One of Long COVID’s Worst Symptoms Is Also Its Most Misunderstood,” quoted the experience of Hannah Davis, a longtime COVID patient and co-author of the paper authored by Eric Topol. She related, “Moments that had an impact on me no longer seem to be a part of me… It seems like both my life and I are voids.”
Joanna Hellmuth, a neurologist at the Public University in San Francisco, told The Atlantic:
At its core [brain fog] is almost always a disorder of “executive function”—the set of mental abilities that includes focusing attention, holding information in mind, and blocking out distractions. When these abilities fail, a large portion of a person’s cognitive structure also fails because they are so fundamental.
A research paper published in Nature in By comparing magnetic resonance imagining (MRI) brain scans of individuals before and after contracting COVID, Gwenaëlle Douaud, Associate Professor at the Nuffield Department of Clinical Neuroscience, published her findings in March 2022. They discovered that the brain had shrunk even with minor infections due to a decrease in the amount of grey matter. The neurons in this area of the brain are important for controlling movement, memory, and emotions.
Douaud noted importantly:
[The participants who were infected experienced a stronger overall decline in the thickness of the grey matter throughout the entire cortex, but this effect is especially pronounced in the olfactory system (related to smell). When comparing hospitalized and non-hospitalized cases, there is also a clear atrophy of the fronto-parietal (involved in sustained attention, complex problem-solving, and working memory) and temporal (associated with processing auditory information and with the encoding of memory) regions, indicating that there is increased damage in the less mild cases.
There is no clear explanation for how SARS-CoV-2 affects the brain. Despite the fact that the virus is known to infect the central nervous system, this is not regarded as an effective, persistent, or common infection.
According to a theory put forth by scientists, the virus does not directly infect the brain but rather disrupts cells known as microglia by inflammatory cells that can travel from the lungs to the brain. Located in the central nervous system (CNS), these cells are macrophages, a subtype of white blood cell. They eliminate diseased neurons and combat infections.
A study published last July in the journal Cell, led by researcher The brain fog that Long COVID sufferers experience is comparable to chemo fog, a syndrome of cognitive impairment brought on by cancer chemotherapy, according to research by Anthony Fernandez-Castañeda of the Department of Neurology and Neurological Sciences at Stanford University.
Fernández-Castañeda noted:
Following mild respiratory COVID, we looked at the mouse hippocampus, a part of the brain involved in memory and learning. We discovered that at seven days after infection, there was a marked increase in microglial/macrophage reactivity in the hippocampal white matter, which persisted for at least seven weeks. An abrupt decline in the production of new neurons was visible seven days after infection and persisted for at least seven weeks, which is in line with earlier findings that reactive microglia and macrophages can inhibit hippocampal neurogenesis.
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), multiple sclerosis, and brain fog are all related, according to neuro-oncologist Michelle Monje, one of the co-authors. She told The Atlantic that neuro-inflammation is “probably the most common way” that COVID-19 causes mental fog.
The Impacts of Long COVID on the Cardiovascular System
At a significant webinar hosted by the World Health Network last September, titled, “The Impact of Long COVID on Health, Society, and Economies,” cardiologist The presentation Rae Duncan gave, which was devastating, was on the long-term effects of COVID-19 on the cardiovascular system.
She related that “COVID is primarily a vascular disease, and Long COVID is no exception. It is a condition that affects all other organs by inducing abnormal blood clotting and inflammation in the blood and blood vessels.”
Duncan cited several studies that show the effects of SARS-CoV-2 infection on the cardiovascular system, including a significant paper written by a top Long COVID researcher and his team in February 2022. The study examined a US Department of Veterans Affairs national health care database identifying a cohort of 153,760 individuals with COVID-19 who were re-examined after one year, finding that the cohort had “increased risks” of cardiovascular disease after 30 days of being infected.
The risks were evident “regardless of age, race, sex and other cardiovascular risk factors, including obesity, hypertension, diabetes, chronic kidney disease and hyperlipidemia (high cholesterol).” People who had no prior history of cardiovascular diseases were particularly at risk.
After one year, they reported that “our results show that 1-year risks and burdens of cardiovascular diseases among those who survive the acute phase of There are many cardiovascular disorders covered by COVID-19.”
According to the study, there is a higher risk of heart attack, heart failure, stroke, acute coronary syndrome, myocarditis (heart muscle inflammation), pulmonary emboli (pulmonary artery blockage), and other conditions. Young patients with no underlying medical conditions also faced similar elevated risks.
Duncan also discussed a research paper from the Journal of the Society for Cardiovascular Angiography & Interventions by Odayme Quesada and her team from Christ Hospital in Cincinnati looked at 585 patients who had COVID-19 infection and STEMI (heart attack brought on by blockage of a heart artery). The study discovered that a significant increase from pre-COVID figures was seen in the percentage of women and men with STEMI who had MINOCAS (myocardial infarction with nonobstructive coronary arteries, a heart attack without artery obstruction).
Research published in a July 2021 study in The Lancet by Data from 86,742 individuals who had contracted COVID-19 in Sweden were examined by Ioannis Katsoularis and his team from the department of Public Health and Clinical Medicine in Ume, Sweden. The researchers pointed to some of the possible causes of SARS-CoV-2 infection on the cardiovascular system:
Through downregulation of the ACE2 receptor, platelet activation, hypercoagulability (increased blood coagulation), and effects on endothelial cells (activation, injury, dysfunction, and apoptosis (cell death)), the exaggerated inflammatory response (cytokine storm) and the direct effect of the virus on endothelial cells (cells that line the blood vessels) are likely to trigger cardiovascular events. The long-term effects of COVID-19 on cardiovascular risk could also be problematic, but further research is necessary.
Further research cited by Duncan published last September in the journal Nature Medicine by scientists from the By Valentina O. Frankfurt, Germany’s Institute for Experimental and Translational Imaging. Putman and her team looked at 346 people who had been infected with the virus at a median of 109 days after infection and were monitored for about 329 days after infection. For a better understanding of the effects post-infection, they looked at non-hospitalized people with no comorbidities in the past.
After the initial period, they found that “structural heart disease or high levels of biomarkers of cardiac injury or dysfunction were rare in symptomatic individuals.” Following up, they discovered that 57% of the subjects had ongoing cardiac symptoms.
The study found that “exertional dyspnea (rapid breathing after mild exertion) was the most frequently experienced cardiac symptom.” They noted that this
manifested as a wide spectrum of exercise intolerance, from the inability to regain a previous level of fitness, climbing stairs or attempting inclines, to the limiting physical aspects of professional or everyday life. Breathlessness was frequently associated with post-exertional exhaustion and an exaggerated tachycardia response (heart rate over 100 beats per minute). Due to sudden onsets of general physical weakness, dizziness, or even blackouts, the more affected participants avoided leaving their homes.
Cardiovascular magnetic resonance imaging (CMR) was used by the researchers to look at the participants’ hearts. To keep track of the virus’s effects, they employed sophisticated mapping techniques called T1 and T2. Each study participant appeared to have some degree of heart muscle inflammation. They discovered an increase in the myocardial water content as well as heart swelling. Increased water content in heart tissue is a sign that heart failure may develop.
Duncan issued a warning that myocardial inflammation could still exist in people who had not experienced an acute, serious infection. She went on to warn that there is “evidence that we may have a bigger problem and that we may have a risk of longer-term cardiovascular complications mediated through endothelial disfunction.”
Duncan urged urgent additional research to establish whether or not post-COVID endothelial dysfunction is improving. She concluded with an alarming warning, stating, “605 million people in the world have been infected with COVID. If the endothelial dysfunction does not resolve on its own, I am extremely concerned that over the next few decades, we will experience a tsunami of cardiovascular complications, such as heart attacks, strokes, and vascular dementia.”
Importantly, Duncan criticized the removal of all COVID-19 mitigation measures by governments all over the world as she concluded her presentation.
Reinfections and the “forever COVID” Strategy
The important scientific work conducted by Ziyad Al-Aly and his team at Washington University School of Medicine deserves special attention. Their body of work emphasizes the ongoing risks to humanity brought on by the criminal pandemic policies of the ruling elites. By allowing COVID-19 to spread unchecked, the virus continues to evolve into new variants that cause recurring waves of mass infections and reinfections, what the WSWS has correctly termed the “forever COVID” strategy.
Al-Aly published a significant study in November of last year that concentrated on the risks of COVID-19 reinfections, which have become more frequent since the Omicron variant first emerged in November 2021.
In the most recent Al-Aly study, 5,693,208 participants totaled 257,427 first-time infected individuals, 38,926 repeat infected individuals, and 5,396,855 uninfected controls. The researchers found that the “risk and burden of all-cause mortality and the prespecified health outcomes increased in a graded fashion according to the number of infections (that is, risks were lowest in people with 1 infection, increased in people with two infections, and were highest in people with 3 or more infections).”
The study notes that these dangers affect both the unvaccinated and vaccinated, stating:
we show that compared to people with first infection, reinfection contributes additional risks of all-cause mortality, hospitalization, and adverse health outcomes in the pulmonary and several extrapulmonary organ systems (cardiovascular disorders, coagulation and hematologic disorders, diabetes, fatigue, gastrointestinal disorders, kidney disorders, mental health disorders, musculoskeletal disorders, and neurologic disorders); the risks were evident in those who were unvaccinated, had 1 shot, or 2 or more shots prior to the second infection; the risks were most pronounced in the acute phase, but persisted in the post-acute phase of reinfection, and most were still evident at 6 months after reinfection.
This study, the most thorough to date on the health effects of repeated infections with COVID-19, makes it clear that each subsequent wave of widespread infection with new SARS-CoV-2 variants will result in an increase in the number of people with Long COVID. For the foreseeable future, the number of patients experiencing heart attacks, strokes, kidney disease, neurological disorders, and other conditions linked to prior COVID-19 infections will continue to rise, placing an undeniable burden on health systems.
Commenting on the long-term impacts that COVID-19 will continue to have on global society, Al-Aly told the Financial Times, “This won’t go away in a week, a year, two years, or three years. This will have an impact on us for many years.”